Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Ocular Presentation of Behcet’s Syndrome Associated with Covid-19 Vaccination
*Corresponding author: Voichanski Shilo, Shaare Zedek Medical Center, Jerusalem, Israel.
Received: February 02, 2022; Published: March 24, 2022
DOI: 10.34297/AJBSR.2022.15.002173
Abstract
Purpose: To shed some light on the long debate as to whether autoimmune diseases might also be triggered by vaccines, through the immune cross-reactivity mechanism.
Observations: We report a case of bilateral pan uveitis and vasculitis, being a first presentation of Behcet syndrome in a young healthy patient who received COVID-19 vaccine. The vaccine might have triggered de novo ocular inflammatory process or ocular exacerbation of an impending Behcet disease, through the immune cross-reactivity mechanism. The patient was treated with oral prednisone and azathioprine with good response. Conclusions and Importance: In our case it might be due to de novo ocular inflammatory process or due to ocular exacerbation of an impending Behcet disease, both might have been triggered by the COVID-19 vaccine the patient received It is important for clinicians to be aware of the association we encountered, and for future post-marketing studies of COVID-19 vaccine to address it.
Conclusions and Importance: In our case it might be due to de novo ocular inflammatory process or due to ocular exacerbation of an impending Behcet disease, both might have been triggered by the COVID-19 vaccine the patient received It is important for clinicians to be aware of the association we encountered, and for future post-marketing studies of COVID-19 vaccine to address it.
Keywords: Behcet’s Syndrome; COVID-19 Vaccination
Introduction
The incidence of uveitis after vaccination is reported to range from 8 to 13 in 100000 persons/year [1]. Several vaccines have been implied to cause uveitis including those against influenza, varicella zoster, diphtheria-tetanus-pertussis, Bacillus Calmette- Guérin (BCG), hepatitis B, hepatitis A, brucella, Human Papilloma Virus (HPV), pneumococcus, and Measles-Mumps-Rubella (MMR) [2]. Vaccination can induce all types of uveitis including specific ocular syndromes such as Multiple Evanescent White Dot Syndrome (MEWDS), Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE), or Vogt-Koyanagi-Harada (VKH), vasculitis, and pan uveitis [3-9]. Three mechanisms have been proposed for vaccine-induced uveitis, by perpetuation of the immune system [10]. Recrudescence of a previously quiet inflammation was reported in after some immunizations, suggesting that a vaccine might not only trigger de novo inflammatory processes but also exacerbate pre-existing inflammation [11]. The COVID-19 has spread worldwide, leading to an ongoing pandemic, necessitating global vaccination programs on the rapid timeline and scale of COVID 19 infections during 2020. Israel leads the world in COVID-19 vaccinations and has vaccinated nearly 40% of its population in just over two months. It has almost exclusively been using the two- shot COVID-19 vaccine developed by Pfizer and BioNTech, which is composed of nucleoside-modified Messenger Ribonucleic Acid (mRNA) (modRNA) encoding a mutated form of the spike protein of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The COVID-19 vaccines have not so far caused worrisome side effects related to vision and have not so far been implicated.
Case Report
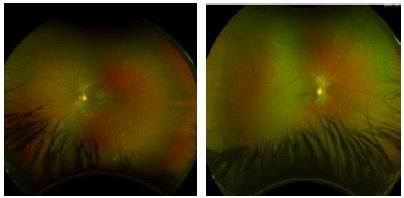
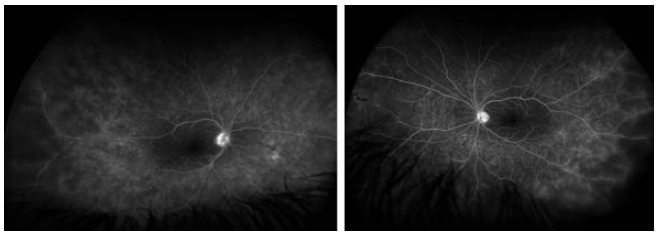
We report on a healthy 20-year-old male who developed photophobia and visual disturbances 10 days after receiving the first dose of Coronavirus disease 2019 (COVID-19) vaccine injection. In addition, he developed a few aphthous ulcers, and a pseudo folliculitic rash appeared on his back with acneiform nodules. Upon presentation, ophthalmic examination revealed bilateral corneal Keratic Precipitates (KPS), cells and flare in anterior chamber. Fundoscopy showed bilateral vitritis, bilateral mild retinitis and mild signs of vasculitis in both eyes, including focal perivascular sheathing and intraretinal infiltrates (Figure 1). Fluoresceine Angiography (FA) demonstrated bilateral temporal peripheral vascular wall attenuation and perivascular hyper fluorescence, suggesting capillary leakages. There was also a small peripheral temporal area of capillary non-perfusion, with no signs of retinal neovascularization (Figure 2). Work up for infectious and inflammatory diseases was inconclusive. Skin pathergy test was negative. The patient was found positive to Human Leukocyte Antigen B51 (HLA-B51). There were no other organ systems involved in the disease. Our patient had bilateral pan uveitis with signs of vasculitis upon presentation. He was diagnosed with Behcet disease based on the International Study Group Criteria (1990) due to his ocular presentation, oral ulcers, and pathognomonic skin lesions. No other underlying disease had been found. He was treated with oral prednisone. A follow up over 3 weeks showed significant clinical improvement with resolution of inflammatory signs in the anterior chamber and vitreous, and improvement of vasculitis signs in both eyes. Prednisone was tapered to a lower dose, and azathioprine treatment was initiated for a long-term effect. A follow-up over 6 months was uneventful.
Discussion
Behcet disease is a systemic vascular disease that can affects a variety of organ systems. Ocular manifestations carry the most serious implications, affecting roughly 70% of patients [12]. The severity is due to recurrent nature of the uveitis, which can lead to permanent, often irreversible, ocular tissue damage. The most significant damage is due to retinal vasculitis, which can cause vascular occlusions, hemorrhages, and macular edema, with significant visual loss [13]. There were previous reports of Behcet disease exacerbation following other vaccinations, like Typhoid [14] and Pneumococcal polysaccharide [15]. Our patient is a previously healthy young individual, who presented with a new onset of bilateral pan uveitis and vasculitis, combined with a previous history of oral ulcers, and late appearance of skin lesions. Ocular disease is the first presentation in only 10-20% of Behcet cases [16]. In our case it might be due to de novo ocular inflammatory process or due to ocular exacerbation of an impending Behcet disease, both might have been triggered by the COVID-19 vaccine he received. In our case, the diagnosis and treatment prevented further development of Behcet extra ocular manifestations. The association between infection and autoimmune disease has stimulated a long debate as to whether such diseases might also be triggered by vaccines, through the immune cross-reactivity mechanism [17].
Conclusion
Several cases associating uveitis with vaccination have been published in the past, but no association has yet been suggested considering the newly authorized COVID-19 vaccine. With ongoing vaccination efforts worldwide, it is important for clinicians to be aware of the association we encountered, and for future postmarketing studies of COVID-19 vaccine to address it.
Patient Consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Declarations
a. Ethics approval and consent to participate- Not applicable.
b. Consent for publication- Not applicable.
c. Availability of data and material- Not applicable (patient’s
anonymity is protected, patient presented is unidentifiable).
d. Competing interests - The authors declare that they have no
competing interests.
e. Funding - None.
f. Author’s contributions - SV was first to examine the patient
and suggesting diagnosis, analyzed and interpreted the patient
data, and wrote the manuscript. BS followed and treated the
patient and was a major contributor in writing the manuscript.
All authors read and approved the final manuscript.
Acknowledgments and Disclosures
a. Funding- No funding or grant support
b. Competing interests - The authors declare that they have no
competing interests.
c. Conflicts of interest - The following authors have no financial
disclosures: SV, BS
d. Authorship: All authors attest that they meet the current ICMJE
criteria for Authorship.
Acknowledgements: None
References
- Agarwal M, Dutta Majumder P, Babu K, Konana VK, Goyal M, et al. (2020) Drug-induced uveitis: A review. Indian J Ophthalmol 68(9): 1799-1807.
- Benage M, Fraunfelder FW (2016) Vaccine-Associated uveitis. Mo Med 113(1): 48-52.
- Gonome T, Suzuki Y, Metoki T, Takahashi S, Nakazawa M (2016) Acute posterior multifocal placoid pigment epitheliopathy and granulomatous uveitis following influenza vaccination. Am J Ophthalmol Case Rep 4: 60-63.
- Braunstein D, Bilha A (2015) Acute posterior multifocal placoid pigment epitheliopathy following influenza vaccination. Rom J Ophthalmol 59(1): 52-58.
- Abou Samra A, Tarabishy AB (2019) Multiple evanescent white dot syndrome following intradermal influenza vaccination. Ocul Immunol Inflamm 27(4): 528-530.
- Blanche P, Decrette C, Sicard D (1994) Development of uveitis following vaccination for influenza. Clin Infect Dis 19(5): 979.
- Wells MB, Garg S (2009) Bilateral panuveitis after influenza vaccination. Retin Cases Brief Rep 3(4): 386-387.
- Tao Y, Chang LB, Zhao M, Li X (2011) Two cases of exudative retinal detachment and uveitis following H1N1 influenza vaccination. Chin Med J (Engl) 124(22): 3838-3840.
- Kim M (2016) Vogt-Koyanagi-Harada syndrome following influenza vaccination. Indian J Ophthalmol 64(1): 98.
- Cunningham ET, Moorthy RS, Fraunfelder FW, Zierhut M (2019) Vaccine-associated uveitis. Ocul Immunol Inflamm 27(4): 517-520.
- Knopf HL (1991) Recurrent uveitis after influenza vaccination. Ann Ophthalmol 23(6): 213-214.
- Ozdal PC (2020) Behçet's Uveitis: Current Diagnostic and Therapeutic Approach. Turk J Ophthalmol 50(3): 169-182.
- Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Meri Urgancioglu (2004) Uveitis in Behçet disease: An analysis of 880 patients. Am J Ophthalmol 138(3): 373-380.
- Molloy ES, Powell FC, Doran MF, Ryan JG, Mulligan NJ, et al. (2004) An unusual case of Behçet's syndrome: triggered by typhoid vaccination? Clin Exp Rheumatol 224(4): 71-74.
- Saeidinejad M, Kardash S, Connell L, (2018) Behcet's disease and severe inflammatory reaction to 23-valent pneumococcal polysaccharide vaccine: a case report and review of literature. Scott Med J 63(4): 119-121.
- Kahirallah M, Accorinti M, Muccioli C, Kahloun R, Kempen J (2012) Epidemiology of Behcet disease. Ocul Immunol Inflamm 20(5): 324-335.
- Vadala M, Poddighe D, Laurino C, Laurino B (2017) Vaccination and autoimmune diseases: is prevention of adverse health effects on the horizon? EPMA J 8(3): 295-311.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.